Acupuncture & Tuina : Osteopathy and Functional Medicine – the synergy between East and West – part 01
“The object of a physician is to find health; any darn fool can find disease”. This could easily be attributed to an ancient Chinese sage-physician (although the use of “darn” gives it away!!) but it was in fact attributed to A.T. Still, the founder of Osteopathy, back in the 1870’s (AACOM, 2022).
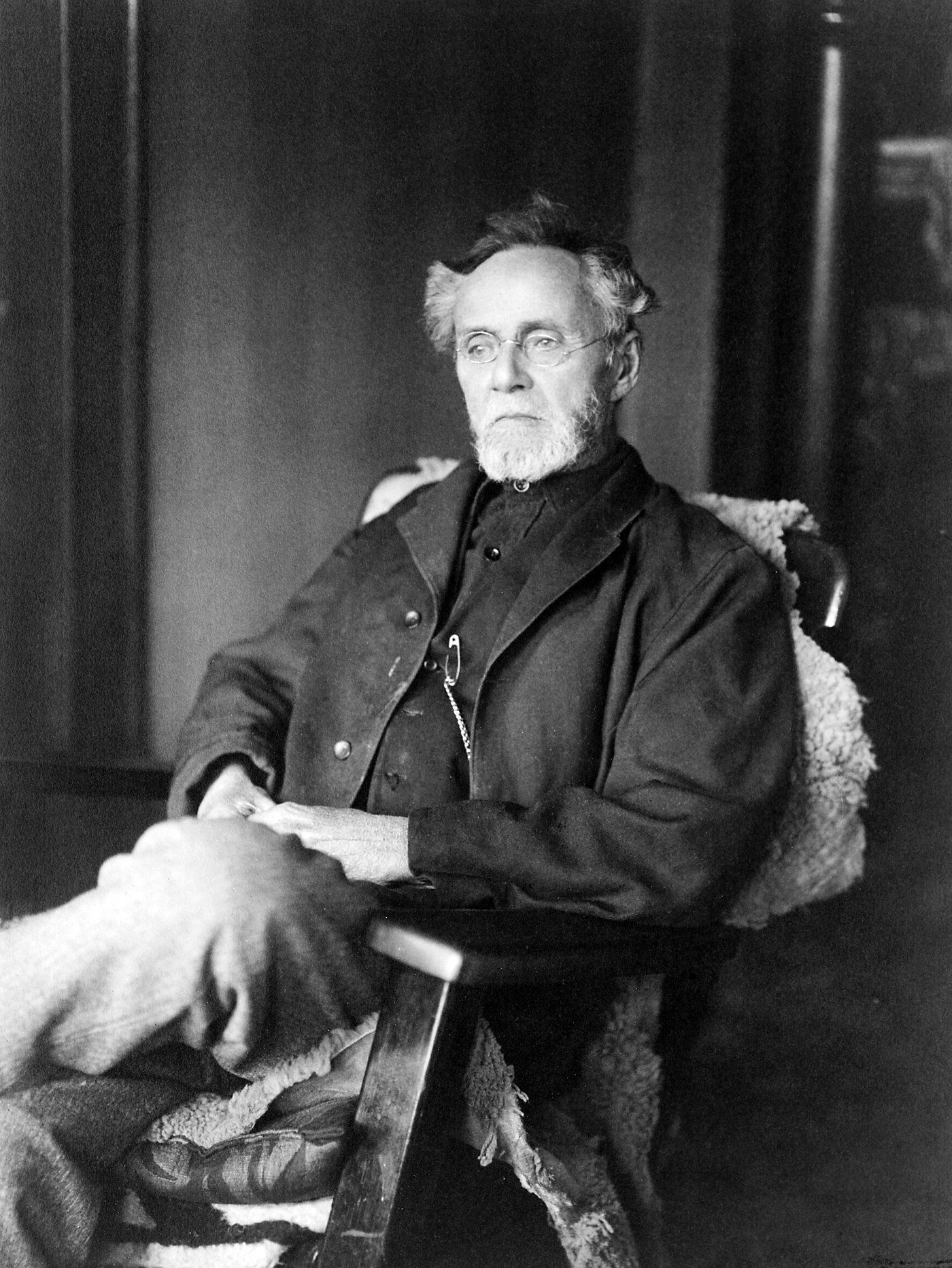
Unknown (Library of Congress collection), Public domain, via Wikimedia Commons
https://upload.wikimedia.org/wikipedia/commons/e/ed/Andrew_Taylor_Still_1914.jpg
Classically Acupuncture and Tuina (not Tuna!!) are 2 of the 4 legs of Classical Chinese Medicine – the other two being herbal medicine and the movement disciplines (including Qi Gong and Tai Qi (link to Tuina page).
People are often surprised when I inform them that I combine these disciplines - however, the more I research and practice, the more I think there are more similarities than differences.
We often forget in the West that until the 18th Century China was probably the most technologically advanced society in the world and Chinese Medicine was the only medicine available to them – and had served them well for well over 2,000 years
A common misconception is that Osteopathy is simply “cracking bones” – in fact Osteopathy was defined as a philosophy, art and science. Osteopathy presupposes that the body unit combines both mind, body and spirit and that no one part works independently of the other – with a healthy body relying on the balance of all three parts. (AACOM, 2022).
Another of the basic tenets of Osteopathy is that health is a natural state and that the human body is a self-healing mechanism and, if left to its own devices, the body will try to heal itself. The viz medicatrix naturae
(lit the healing power of nature), or viz
for short, was initially attributed to Hippocrates, which stated that organisms left alone can often heal themselves (Wikipedia, 2021). Unfortunately, as human beings, we tend to put a spanner in the works by either over-use, under-use or ab-use of our body (see later blogs on movement, nutrition and lifestyle, the Yangsheng
- or nourishing life - principles of Chinese Medicine).
A further principle of Osteopathy is that “the rule of the artery” is supreme and that adequate circulation is paramount for life and the healing process. Chinese Medicine concurs, with the flow of Qi and Blood being necessary for survival and healing.
Another principle of Osteopathy is that both structure and function of the body are inter-related with structure informing function, and function relying on structure (more of this in a later blog) and that a rational treatment is based on the basic principles of body unity, self regulation and the interrelationship of structure and function.
Interview on UK Health Radio on the interplay of East and West healthcare - together with a little about my journey
The Osteopathic principle of viz also incorporates the idea that we are born with a vitalism, a differing amount for each person (their inherent constitution) and that when this fixed amount is used up - we die. This vitalism can be supported by good lifestyle, and can be drained by poor lifestyle. A similar concept was put forward in the 1980,s by Dr James Fries, a professor of medicine at Stamford university. who described the idea of a functional reserve for all the body's organ systems which, in youth, is far greater than the body's needs - a "savings account for extra biological needs". He termed this "compression of morbidity" (Stamford News, 2021).
Professor Jeffrey Bland PhD (often acclaimed as the "father of functional medicine") in his book clarifies this, saying that we can utilise this reserve in times of need e.g. trauma / stress (the stress response of the body allows 4-5 times normal oxygen supply to the vital organs, and our kidneys / liver can detoxify bodily toxins). However, as we age, this functional reserve diminishes - but that lifestyle changes can help retain this organ reserve for as long as possible, thereby reducing the time we spend with chronic illness. He goes on to cite Fries who followed up his 1980 paper in 1998 with the results of a study of 1,741 university alumni who were followed since 1962 (average age 43). The results of this study showed that those who followed high-risk lifestyle behaviour experienced twice the cumulative disability and the lower risk group postponed the first onset of disability by 5 years (Bland 2015)
My Chinese Medicine and Applied Channel Theory teacher, Prof Wang Ju-Yi stated that, after 50 years of clinical practice and study, the following expression summerised his views on Chinese Medicine and Acupuncture:
- "The 5 Zang (organs) foster essence thus govern destiny" - our inherited constitution (or essence) gives us our pre-disposition which is supported by organ function - cultivation of this is necessary for life and to fulfill our potential destiny. Disciplines like Yoga / Tai Qi. and lifestyle advice, following the yangshen principles, help us prolong this. He goes on to say that;
- "The "channel system permeate, thus govern life" (Wang Jy-Yi, 2013). What is actually achieved in acupuncture is to regulate the channels to allow the body to heal itself (see a later blog on the 5 Zang organs and the channel system). For further information on Prof Wang (including articles and podcasts) - click here
According to Dr David Miller (2020) a common criticism in the West is that Traditional / Classical Chinese Medicine is “unscientific”. However, he points out that Chinese Medicine is “observational biology and that it does follow a scientific process - it:
1. Observes a phenomenon – it gathers knowledge of pathology (signs and symptoms of a disease process). It then;
2. Formulates a Hypothesis to explain the phenomena, using the scientific terminology of the period. It then;
3. Predicts other phenomena by use of this hypothesis. Finally, it;
4. Confirms the results by the performance of test – literally undertaken by several thousand experimenters (Chinese Medicine Practitioners) over thousands of years to billions of patients.
It is impossible to directly equate Western and Chinese medicine, as they come from different historical views on how the body-system works. However, as you can see many of the philosophical and practical roots of Osteopathy and Chinese Medicine are not dissimilar, and I personally believe that their differences are outweighed by their similarities.
References
AACOM (2022) American Association of Colleges of Osteopathic Medicine – The Philosophy of Osteopathy. Found on https://www.aacom.org/become-a-doctor/about-osteopathic-medicine/philosophy-tenets-of-osteopathic-medicine
Bland J (2015) The Disease Delusion - conquering the causes of chronic illness for a healthier, longer and happier life, Harper Collins,
Stamford News (2021) Stamford Medicine Professor James Fries, a proponent of healthy medicine, dies at 83. Found on https://med.stanford.edu/news/all-news/2021/12/james-fries-obituary.html
Wang, Ju Yi (2013) Applied Channel Theory in Practice, Found on https://www.channelpalpation.org/theory
Wikipedia (2021)
The Viz medicatrix naturae, found on https://en.wikipedia.org/wiki/Vis_medicatrix_naturae
If you have a spare hour or so look at the “Introduction to Traditional Chinese Medicine” video below by Dr David Miller MD, L..Ac (a Western Medical Doctor and Acupuncture Practitioner) where he explains these concepts to a groups of Medical Students from Harvard Medical School.








